Autoimmune hemolytic anemia (or autoimmune haemolytic anaemia; AIHA) happens when antibodies led from the individual’s own red blood cells (RBCs) make them burst (lyse), resulting in an inadequate amount of oxygen-carrying red blood cells from blood flow. The duration of this RBCs is decreased from the regular 100–120 days to only a couple of days in severe circumstances. The intracellular elements of the RBCs are introduced into the circulating bloodstream and to cells, resulting in a number of the characteristic signs of the illness. The antibodies are often directed against high-incidence antigens, so additionally they generally act on allogenic RBCs (RBCs originating from beyond the individual themselves, e.g. in the event of a blood transfusion). AIHA is a relatively rare condition, affecting one to 3 individuals per 100,000 annually.
The language employed in this disorder is somewhat ambiguous. Though MeSH utilizes the expression “autoimmune hemolytic anemia”. Some sources favor the expression “immunohemolytic anemia” so medication reactions could be included within this category.
Causes of Autoimmune Hemolytic Anemia
The causes of AIHA are poorly understood. The disease might be primary, or secondary to a different underlying illness. The main disease is idiopathic (the two phrases used synonymously). Idiopathic AIHA accounts for roughly 50 percent of instances. Secondary AIHA could result from a number of different ailments. Warm and cold kind AIHA each have their very own more prevalent secondary causes. Less frequent causes of warm-type AIHA contain neoplasms aside from lymphoid, and disease. Exotic cold form AIHA can also be caused chiefly by lymphoproliferative disorders, but is also generally brought on by disease, notably by mycoplasma, viral disease, infectious mononucleosis, and other respiratory ailments. Less commonly, it may be brought on by concomitant autoimmune ailments.
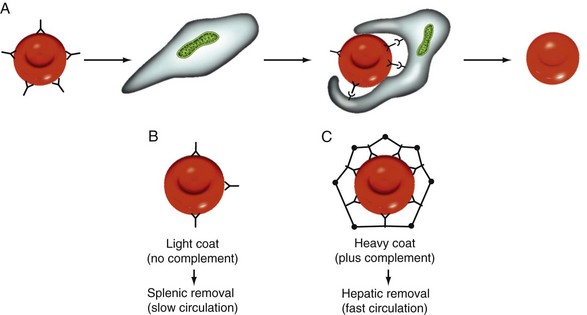
Drug-induced AIHA, although infrequent, can be brought on by numerous medications, such as α-methyldopa and penicillin. This can be a type II immune reaction where the drug binds to macromolecules on the surface of the RBCs and functions as an antigen. Antibodies are created from the RBCs, which contributes to complement activation. Complement objects, such as C3a, C4a and C5a, trigger granular leukocytes (e.g., neutrophils), though other elements of this machine (C6, C7, C8, C9) either could form the membrane attack complex (MAC) or may bind the antibody, helping phagocytosis by macrophages (C3b). This is 1 kind of “penicillin allergy”.
Treatment of Autoimmune Hemolytic Anemia
Much literature exists concerning the treatment of AIHA. Efficacy of therapy is dependent upon the right identification of either warm- or cold-type AIHA.
Warm-type AIHA is generally a more insidious disorder, not treatable simply by eliminating the underlying cause. Corticosteroids are first-line treatment. For people who don’t respond or have recurrent disease, splenectomy may be contemplated.
Cold agglutinin disease is treated together with avoidance of cold exposure. Patients with more severe disease (symptomatic anemia, transfusion addiction) could be treated with rituximab. Steroids and splenectomy are somewhat less efficacious in cold agglutinin disease.
Paroxysmal cold hemoglobinuria is treated by eliminating the underlying cause, such as disease.