Esophageal varices (occasionally spelled oesophageal varices) are very dilated sub-mucosal veins at the lower third of their esophagus. They’re most often a result of portal hypertension, generally because of cirrhosis; patients with esophageal varices have a powerful inclination to develop bleeding. Esophageal varices are generally diagnosed via an esophagogastroduodenoscopy.
The top two thirds of this esophagus are emptied through the varicose veins, which carry deoxygenated blood in the esophagus into the azygos vein, which then drains right into the superior vena cava. These veins don’t have any role in the progression of esophageal varices. The lower one third of the esophagus is emptied into the shallow veins liner that the bronchial mucosa, which divides into the left gastrointestinal tract (coronary artery), which then drains right into the portal vein. These superficial veins (normally only about 1 millimeters in diameter) become swollen into 1–2 cm in diameter in connection with portal hypertension.
Prevention of Esophageal Varices
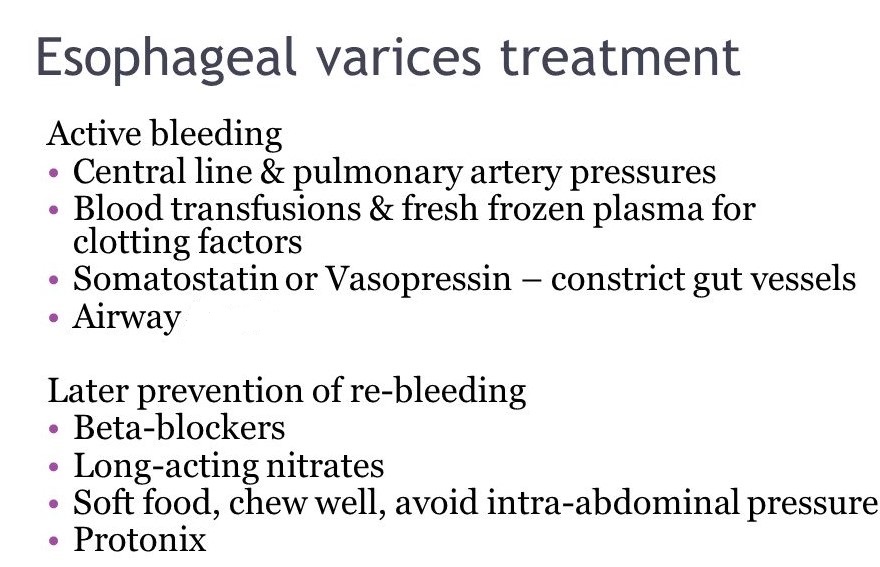
In ideal conditions, patients with known varices should get treatment to decrease their risk of bleeding. The non-selective β-blockers (e.g., propranolol, timolol or nadolol) and nitrates (e.g., isosorbide mononitrate (IMN) are assessed for secondary prophylaxis. Non-selective β-blockers (although maybe not cardioselective β-blockers such as atenolol) are favored since they reduce equally cardiac output by β1 blockade and splanchnic blood flow by obstructing vasodilating β2 receptors in splanchnic vasculature. The efficacy of the treatment was proven by a variety of different research studies.
But, non-selective β-blockers don’t stop the formation of esophageal varices.
When medical contraindications into beta-blockers exist, for example important reactive airway disorder, then treatment with prophylactic endoscopic variceal ligation is frequently done.
Treatment of Esophageal Varices
In crisis situations, care is aimed at stopping blood flow, keeping plasma volume, adjusting disorders in coagulation caused by cirrhosis, and proper utilization of antibiotics like quinolones or ceftriaxone. Blood volume resuscitation needs to be carried out immediately and with care. The goal ought to be hemodynamic equilibrium and hemoglobin of more than 8 g/dl. Resuscitation of all lost blood contributes to rise in portal pressure resulting in more bleeding. Volume resuscitation may also worsen ascites and boost portal pressure.
Therapeutic endoscopy is regarded as the mainstay of urgent therapy.
Therapeutic endoscopy is considered the mainstay of urgent treatment. The two main therapeutic approaches are variceal ligation or banding and sclerotherapy.
In cases of refractory bleeding, balloon tamponade using a Sengstaken-Blakemore tubing could be mandatory, generally as a bridge to additional endoscopy or therapy of the root cause of bleeding (generally portal hypertension). Esophageal devascularization surgeries like the Sugiura processmay also be employed to prevent complicated variceal bleeding. Techniques of treating the portal hypertension include: transjugular intrahepatic portosystemic shunt, or even a distal splenorenal shunt process or a liver transplantation.



