In these days of rising healthcare costs, it’s not often that a medical test or procedure offers two benefits for the price of one.
But researchers have discovered that women who get a routine mammogram to screen for breast cancer may soon get a bonus: screening for coronary artery disease.
In a study presented at the American College of Cardiology (ACC) annual scientific sessions March 24, and soon to be published in the Journal of the American College of Cardiology Imaging, researchers say thatroutine mammograms also show hardened cholesterol in the arteries.
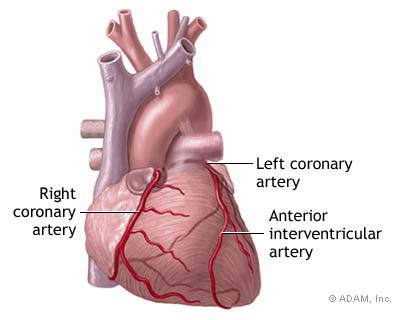
“Arteries supply the breasts with nutrition the same way they supply our heart, our brain, our feet, and everywhere else,” explains lead study author Laurie Margolies, MD, director of breast imaging at Mount Sinai Hospital and an associate professor of radiology at Mt.
Sinai’s Icahn School of Medicine in New York City. “The hardening of the arteries, or atherosclerosis, can affect the arteries in the breast just the same way it can affect the heart and the brain.”
Mammograms are designed to identify calcifications — the buildup of calcium salts — because calcifications may indicate early cancer, Dr. Margolies says.
While looking for those potentially cancerous calcifications, radiologists may also see a different kind of calcification caused by cholesterol buildup in breast arteries.
Calcifications in the arteries will show up as parallel lines instead of the irregular patterns seen in calcifications that may indicate cancer in breast tissue.
Margolies and her colleagues wondered whether identifying those parallel lines could help doctors determine women’s risk for coronary artery disease.
The researchers compared radiography results from 292 women who had not already been diagnosed with coronary artery disease.
All of the women had gotten a mammogram and a CT scan of the chest within the same year.
CT scans had been done for a variety of routine reasons not necessarily related to cardiovascular concerns.
Each woman had enough information in her chart for the researchers to analyze risks for atherosclerosis or heart disease.
How Mammograms and Other Heart Disease Screenings Compare
The researchers used the women’s risk factors to calculate two measures that physicians often use to determine how likely someone is to develop hardened arteries or heart disease.
One is the risk assessment tool from the Framingham Heart Study, which uses your age, sex, total and HDL cholesterol levels, smoking status, systolic blood pressure, and use of any blood pressure-lowering medications to calculate risk.
The other, the ASCVD risk estimator, uses the same information while also considering a person’s race and whether they have diabetes.
The researchers found calcifications in the breast arteries of 43 percent of the women.
The likelihood of having these calcifications increased with age, as well as among those with high blood pressure and chronic kidney disease.
Having these calcifications correctly identified women with atherosclerosis 63 percent of the time.
About one-quarter of the women whose mammograms didn’t show hardening in the breast arteries actually did have atherosclerosis.
Together, the researchers say, these results mean that mammography was 70 percent accurate at identifying women with hardening of the arteries in this study.
For comparison, when they looked at the women’s Framingham risk score, they found a 55 percent overlap of atherosclerosis risk based on that score and risk based on having calcifications in breast arteries.
Similarly, the overlap with the other pooled cohort equation was 54 percent.
“What we are presenting and advocating for is a successful way, with no extra money or extra radiation, of determining a woman’s risk of cardiovascular disease at the same time she would be screened for breast cancer,” Margolies says. “It’s really a revolutionary way to assess cardiovascular risk in breasts, because you’re screening for breast cancer and cardiac disease at the same time.”
What You Can Do About Heart Disease Risk
Although getting heart-risk information from mammograms could be helpful, you shouldn’t seek a mammogram for the purpose of determining your heart disease risk, points out Sarah Samaan, MD, a cardiologist at the Heart Hospital Baylor in Plano, Texas.
“The major risk factors continue to be hypertension, high cholesterol, diabetes, smoking, family history, an unhealthy diet, and a sedentary lifestyle,” Dr. Samaan says. “A regular checkup with your doctor is your best first line of screening.”
Women with a higher risk for heart disease can have a coronary calcium scan, which looks for calcifications in heart arteries.
But this test is not routinely recommended in women under age 50 unless they’re very high-risk, because it involves twice the radiation of a mammogram, Samaan says.
“Women with heart symptoms, like chest pain or shortness of breath, need more detailed cardiac testing, such as stress testing or echocardiography,” she explains. “It’s important to see your doctor if you have any symptoms that occur with exertion, or any concerns about your heart at all.”
Also, it’s important to note that mammograms can’t diagnose atherosclerosis; that’s best done with an invasive procedure called a coronary angiogram, or cardiac catheterization.
For this test, a doctor inserts a catheter into the heart through an artery in the groin or wrist, Samaan says.
But because this procedure costs several thousands of dollars and has a low, but serious, risk of complications, you would only undergo it if your doctor thought you showed clear evidence of blocked arteries in blood tests or other testing, or if you had severe symptoms.
But in the future, your routine mammogram could do double duty as a screening test for heart disease risk.
“The key is that this really is a practice-changing and accessible way of determining risk with no extra radiation and no extra money or extra time,” Margolies says.
“Given that prevention is key for reducing mortality, perhaps this is something we should all be doing and asking for.”
- ByTara Haelle