Even in a developed country like the USA, a recent study showed that patients with vision problems due to diabetes are unaware of diabetes’ effect on the eyes.
A few days ago, a patient from central Kathmandu came to me with gradual loss of vision for a few months. She was from a prosperous family and with a good education.
However, it was quite distressing to know that she had already lost more than half of her sight and that it was not salvageable. Similarly, there was another gentleman from far western area who had been to different eye hospitals.
Finally, when he came to us, his vision in both eyes was completely gone. These stories have become day to day affairs; a reality, which is in fact, could have been easily avoided if people were better informed.
Even in a developed country like the USA, a recent study by Verma R and his associates showed that the patients with vision problems due to diabetes are unaware of diabetes’ effect on the eyes. Of 286 participants identified as diabetics with vision problems, 70% were not aware that diabetes had affected their eyes; 62% reported not having visited a diabetes specialist in the past year; and 33% reported not receiving a dilated eye exam in the past year.
What is diabetes?
Diabetes is fast becoming a major public health problem worldwide. Unfortunately, very few are aware of problems diabetes can cause to the eyes. According to a survey in 2000, 2.8% of the world population had diabetes.
It is presumed that this disease would affect a total of 4.4% by the end of 2030. It was found that 4.8% of the cases of total blindness are due to the complication of diabetes in the eye.
Diabetes is a lifelong disease that involves problems with the insulin hormone. Normally, the pancreas, a tiny organ behind the stomach, releases insulin to help our body store and use the sugar and fat from the food we eat.
Diabetes occurs when the pancreas does not, or produces very little, insulin. Diabetes affects the entire body, the most organs so affected being the heart, kidney, eyes, feet, and sexual organs.
What are the effects of diabetes in the eye?
1. Infection of the eye: Diabetic patients are more prone to infection as high blood sugar level makes them less resistant to fight against infection.
2. Dryness of the eyes: Diabetics tend to suffer from dry eyes, causing gritty feeling in the eyes.
3. Temporary blurring: High blood sugar level leads to swelling of the lens of the eye, causing inability to see objects clearly.
If you have eye problems and diabetes, do not rush to buy a new pair of glasses immediately, as high sugar level can cause blurred vision. Once your diabetes is stabilized, the vision will clear automatically.
4. Cataract: Fogging or clouding of the normal clear lens of the eye is called cataract. People with diabetes can get such eye problems earlier and can progress more rapidly than in those without diabetes.
The lens inside the eye allows us to see and focus on an image just like a camera. This makes our vision burred, as images cannot pass through the cloudy lens clearly.
However, cataracts can be successfully removed by surgery, and usually it is possible to insert a man-made lens implant.
5. Glaucoma: When fluid inside the eye does not drain properly, it can lead to excess pressure inside the eye and this condition is called glaucoma.
The increase in pressure can damage nerves and the blood vessels in the eye, causing changes in vision. Most of the time, the patient is unaware of any symptoms of glaucoma, like headache, pain of the eye, and haloes around light.
The damage due to this condition is found only during an eye examination. Treatment requires lowering the eyes’ pressure by increasing the drainage of the fluid inside the eye or decreasing the production of the fluid. Eye drops are used for both purposes.
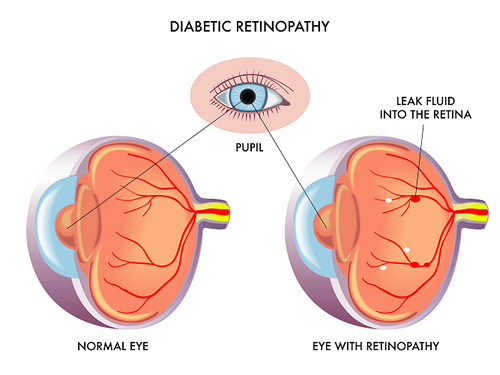
6. Retinopathy: Retinopathy is the medical term for damage to the tiny blood vessels that nourish the retina, the tissue at the back of our eye that captures light and relays information to our brain.
The high blood sugar levels associated with diabetes can easily affect these blood vessels.
What is diabetic retinopathy?
Diabetic Retinopathy: It is the fifth commonest cause of blindness in the world. The longer the duration of diabetes, the greater the risk of this very serious eye problem. If retinopathy is not found early, or is not treated, it can lead to blindness.
Background Diabetic Retinopathy: This condition is very common in people who have had diabetes for a long time. The doctor may be able to see abnormalities in the eyes, but there is no threat to the sight. There are two types of diabetic retinopathy which can damage to sight. Both involve the fine network of blood vessels in the retina. They are described below:
Maculopathy: This happens when the central part of the retina is affected by leaky blood vessels. If the macula is affected, one may find it difficult to recognize people’s faces in the distance or to see detail such as small print.
Proliferative Diabetic Retinopathy: New blood vessels form when blood supply to retina becomes less in the eye. This is a natural way of trying to repair the damage due to diabetes. However, these new blood vessels are very weak and fragile, and as a result, these blood vessels can bleed very easily and cause scar tissue to form in the eye. The scar tissue can pull the retina away from the back of the eye. This is known as retinal detachment, and it can lead to blindness if untreated.
What is its treatment?
Early-stage retinopathy may not need to be treated, but more advanced retinopathy may require laser treatment or injections of medicine into the eye.
One should have the eyes examined every year by an ophthalmologist so the condition can be closely monitored.
An ophthalmologist is a specialist in identifying and treating eye conditions. More advanced stages of retinopathy would require laser treatment if there is a considerable amount of bleeding from the blood vessels in the eye, and in maculopathy, to restore the eyesight. Alternatively, a new treatment for retinopathy, intravitreal anti-VEGF injections, may be recommended.
Laser treatment: The type of laser treatment used to treat diabetic retinopathy is called photocoagulation. Laser photocoagulation uses the heat from a laser to seal or destroy abnormal, leaking blood vessels in the retina. It may not restore vision that has already been lost.
But, when it is done in a timely manner, laser treatment may reduce the risk of future vision loss. It works by sealing any blood vessels that are leaking and destroy any abnormal blood vessels that have grown in the retina.
An ophthalmologist will carry out the procedure, which usually involves one or more visits to a laser treatment clinic. It is an outpatient care, which means the patient will not have to stay in the hospital overnight. During the procedure, the patient will be given a local anesthetic to numb the surface of the eye, and eye drops to widen the pupils.
A special contact lens will be placed on the eye to allow the laser beam to be focused onto the retina. Laser treatment is usually a painless procedure but one may feel a sharp pricking sensation when certain areas of retina are being treated.
Intravitreal anti-VEGF injections: Intravitreal anti-VEGF injections are often used to treat changes at the centre part of the back of the eye, called macula, due to aging changes.
However, research has shown that they can also improve the vision of people with diabetic retinopathy. Intravitreal anti-VEGF injections are given by an ophthalmologist on an outpatient basis.
What are the preventive measures to avoid blindness from diabetes?
1. Early examination of the eyes with eye doctor or ophthalmologist, and early treatment. Early diagnosis is vital, so it is always advisable to go for eye check up when diabetes is diagnosed. Have an eye examination every year and do not wait until the vision has deteriorated to have an eye test. Remember, however, that if the vision is getting worse, this does not necessarily mean one has diabetic retinopathy. It could simply be simply be corrected by glasses.
2. Diabetic retinopathy can be minimized with a combination of strict blood sugar control and routine screening with eye exams.
3. High blood pressure, high blood cholesterol, and obesity are risk factors for diabetic retinopathy and should be treated. Smoking can also worsen the condition. Hence, it is advisable to quit smoking, if possible.
4. Pregnancy can precipitate or worsen retinopathy in women with diabetes who take insulin, so any such woman considering pregnancy should discuss the risks with her doctor.
Finally, an early detection and treatment of retinopathy can prevent many, or even most, cases of severe vision loss and blindness in people who have diabetes.